
Tuberculosis (TB) is the most common opportunistic infection and one of the leading causes of death among people living with HIV(PLHIV) worldwide.
The lifetime risk of developing active TB in a person who is not infected with HIV is about five to 10 percent lower as compared to a person living with HIV.
Globally, the risk of developing active TB is 20 times higher among people living with HIV than those who aren’t. However, around 6,000 patients with active TB are registered every year.
Compared to its immediate neighbors, Rwanda has a relatively low TB incidence, currently at 58 infections per 100,000 people, a steady decrease from 96 infections per 100,000 people in 2000.
TB is caused by a germ called Mycobacterium tuberculosis. The germs are spread from person to person through the air when a person with pulmonary TB coughs, sneezes, laughs, or sings.
TB germs can remain inactive in the lungs for a long period but can still be passed on to others. However, if these germs become active and multiply, the patient will develop TB. These germs usually attack the lungs, but they can also attack any part of the body, such as the kidneys, brain, spine, skin, and others.
TB symptoms include prolonged fever, chronic cough, drenching night sweats and weight loss.
People living with HIV are more likely than others to contract TB because HIV weakens the immune system and causes depletion and dysfunction of CD4 cells making it harder for the body to fight back infection.
The ‘World Health Organization End TB Strategy’ prioritizes preventive treatment among people living with HIV.
Additionally, the 2021 Political Declaration on HIV/AIDS states that to reduce TB-related morbidity and mortality among people living with HIV, 90 percent of them should receive TB preventive treatment.
The Ministry of Health through RBC recommends the implementation of TB preventive therapy to people living with HIV.
While TB vaccination does not prevent infection, it protects many against the most severe forms of tuberculosis (milliary and TB meningitis).
TB vaccination is compulsory for newborns and infants exposed to HIV if they are asymptomatic and infants with signs and symptoms of clinical AIDS.
However, it is recommended that TB vaccination is postponed in premature babies and newborns whose weight is below 2.5 kilograms.
A combination of HIV and TB poses challenges in both the diagnosis and treatment processes.
To increase TB detection in HIV-infected individuals, healthcare providers are advised to screen TB by asking patients if they have been coughing for more than three weeks, have extreme weight loss in the past three weeks, have chest pain, or whether they are having excessive night sweats or have contact with someone who contracted TB.
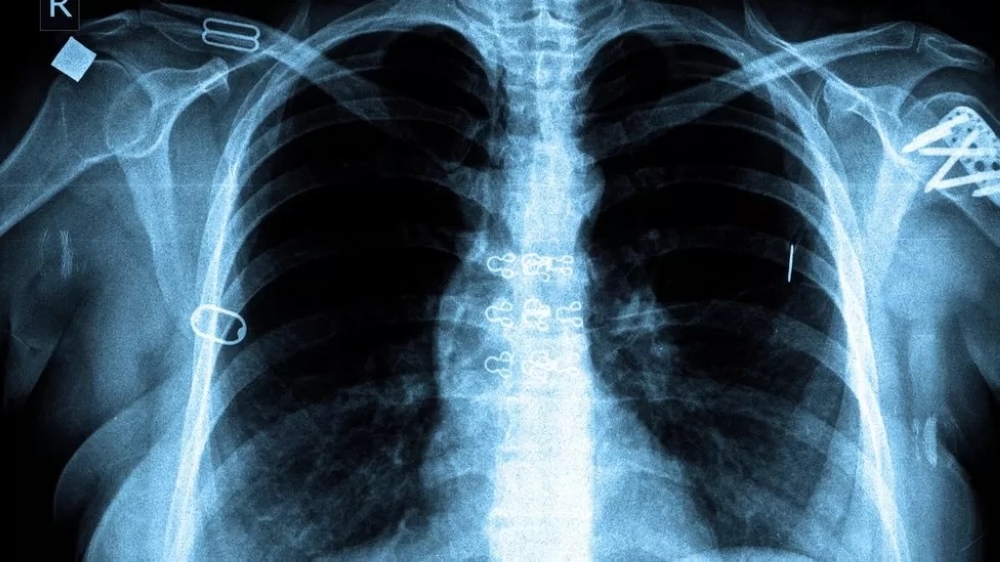
If the patient has any of the above signs, a few exams are done in the laboratory. The laboratory exams include sputum exams, chest x-ray, gen expert, CT scan, and culture from potentially infected organs.
Besides the screening, the government has poured its resources into ensuring the treatment of all persons living with HIV regardless of age as well as identifying those cases who do not know their status.
Additionally, the government provides TB preventive therapy to household contacts of those persons staying with a person with TB.
Currently, across the country, more than 69 GeneXpert using molecular testing technology machines are in use for TB diagnosis in all hospitals and some health centers with high TB rates.
What should you do when you have TB and live with your family?
Once you know you have active TB, take TB drugs right away because you need less than two weeks of consistently taking the medication as prescribed by the doctors to stop spreading the germs.
Ensure that your mouth and nose are always covered with an N95 face mask. You can also try to drink warm liquids to avoid coughing a lot since sneezing and coughing can potentially spread germs.
As a patient, ensure that you spend less time in shared places like seating rooms, dining, bathrooms, and kitchens. The people sharing a home with a patient and the patient himself are advised to regularly wash their hands and wear gloves.
How can you support someone with active TB that shares your home?
It is advisable that the person with active TB is put in a well-ventilated and isolated room seven days before and another seven days after taking TB drugs.
You can provide the patient with some fruits and vegetables like oranges, mangoes, sweet pumpkin, carrots, tomatoes, nuts, and seeds since they are excellent sources of Vitamin A, C, and E which are highly required.
Dr. Julius Kamwesiga, Medical Director, AIDS Healthcare Foundation (AHF)


